St John’s Research Institute and Harvard’s India Digital Health Network, in collaboration with the National Health Authority, are conducting a first of its kind in-depth evaluation of the most pressing needs felt by various stakeholders in India’s health delivery landscape to better target the billions of dollars of investment expected in digital health tools, data science and AI, in the coming years.

Using a generative design research process, our clinicians are meeting with over 150 contributors from across the healthcare spectrum, from community health workers, to relatives of patients, to hospital leaders to venture capitalists. In each interview session, lasting hours, is unearthing conscious and aspirational needs through a collaborative interactive exploration.
Billions have been invested in digital health tools globally in the past decade with poor returns on investment because of a misalignment of priorities between patients, providers, administrators, payers, innovators and investors.
Clinical needs and workflows, and preventive public health interventions have seldom been prioritized, despite significant gains in clinical and population health outcomes, if addressed. The NFS seeks to prioritize areas of shared interest and gaps across this stakeholder ecosystem to guide investment and research priorities in digital health implementation science.
Why Now?
India is uniquely positioned to leverage digital health tools to deliver better health services to its billion plus population.
Three unique features of India’s digital ecosystem will drive this change:
The Government of India’s thrust on Digital Public Infrastructure.
This calls for digital public goods widely available to the population.
Near-universal, and inexpensive cell phone ownership in India.
This allows the vast majority of households to access the internet.
The National Health Authority’s unique ABDM health data architecture.
This allows for API-enabled, patient-centric, patient-controlled, consent-driven data flows, potentially saving India billions in EMR costs.
The philanthropic, private and public sector will invest billions more, given the vast potential for change driven by AI, and especially Large Language Models. It is imperative that we do not repeat the mistakes of the last decade by making blind investments agnostic of the most pressing needs of our patients and clinicians, our health system and public health department leaders, our scientists and educators. Targeting innovation to meet these real world priorities will reap better returns – for all.
Who?
The research is currently being conducted in 9 locations across 5 States of India.
We have collected data from 22 Government health facilities and 17 Private health facilities across the following stakeholder groups:
Community Health Workers
Doctors
Nurses
Allied Health Professionals
Administrators
Patients
Patient Caregivers
DH Companies
The Process
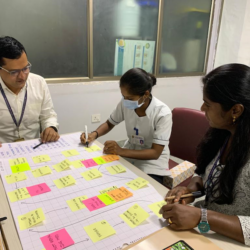
The study adapts generative design research methods and engages with various Indian healthcare stakeholders — including participants in the community, health facilities, and board rooms — to elicit in-depth insights efficiently.
Step One
We first understand what a “day in the life of…” looks like. What are all the tasks a medical officer must perform daily? What are her pain points? What are a grandmother’s daily healthcare needs – taking her medications, remembering to put on her cane? What does she have trouble doing? Why?
Step Two
We then ask them what digital solutions may help them, and if they can imagine what these would look like.
The study uses flowcharts and user-driven prototyping to explore the participants’ present context, past experiences, and dreams for the future. The toolkit includes sticky notes, customized templates, play-dough, and lego blocks to help participants make artifacts that capture their ideas.
Step Three
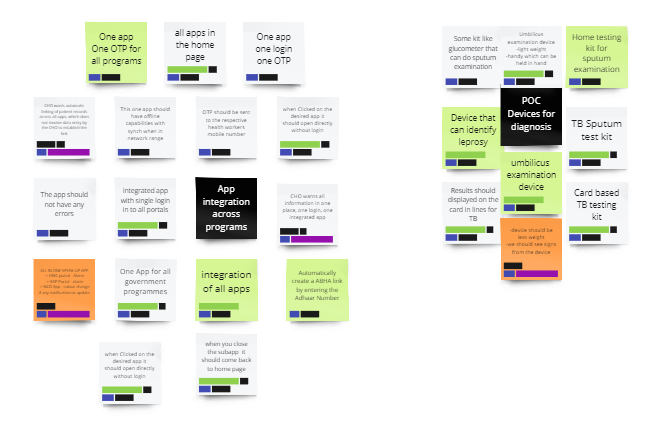
We map our findings onto affinity diagrams to form new insights.
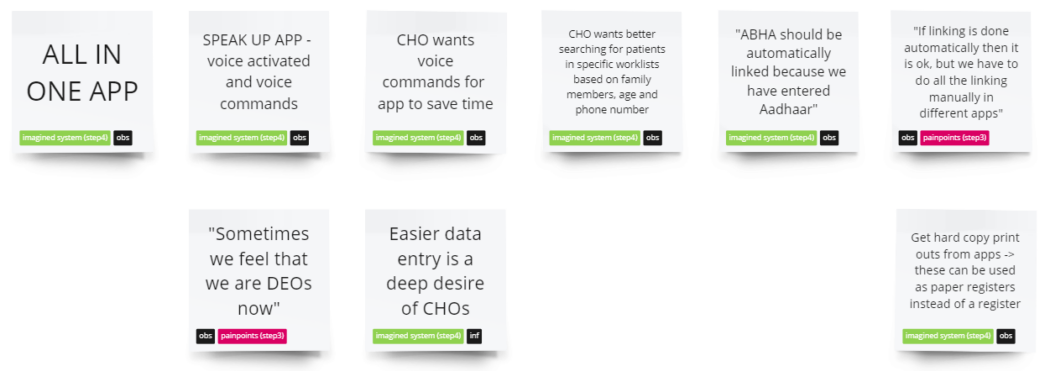
We cluster our insights from across the various stakeholders – what are the common themes in each group? What are the common themes across groups? Where is there no overlap? What is it that the insurance carrier really wants to know, that is not clinically relevant and yet that doctors are made to collect and enter information on? What population health needs do administrators really need to make better investments that ASHA workers have no use for, but are made to collect? The clusters are compared across stakeholder groups and shared themes and needs are identified.
Step Four
Progress
Community Health Workers
Government: 9
NGO: 7
Doctors
Primary Care: 13
Secondary Care: 4
Tertiary Care: 6
Nurses
Toal: 13
Allied Health Professionals
Total: 2
Administrators
Government: 5
NGO: 3
Corporate CIO: 3
Patients
Total: 28
Patient Caregivers
Total: 10
DH Companies
EHR Companies: 2
mHealth Company: 1
Device Company: 3
Quotes from participants about our generative sessions
Team

Dr. Verghese Thomas
St. John’s Research Institute

Dr. Bharat Kalidindi
St. John’s Research Institute

Dr. Abijeet Waghmare
St. John’s Research Institute

Dr. Dhinagaran D
St. John’s Research Institute

Ms. Sruthy Xavier
St. John’s Research Institute

Dr. Panchami VK
St. John’s Research Institute
Mr. Tejesh S
St. John’s Research Institute

Ms. Evangeline Prathiba
St. John’s Research Institute

Dr. Shitij Arora
Montefiore Medical Center, Albert Einstein College of Medicine

Dr. Tony Raj
St. John’s Research Institute

Dr. Satchit Balsari
Harvard Medical School, Beth Israel Deaconess Medical Center
Partnering Institutions




- Govt of Karnataka Department of Health and Family Welfare
- Govt of Meghalaya Department of Health and Family Welfare
- SEWA-Rural, Gujarat
- Basic Health Services, Rajasthan
- St. John’s Medical College and Hospital, Bangalore
- Cura Hospitals, Bangalore
- SAN-KER Hospital, Shillong
- Dr. H. G. Roberts Memorial Hospital, Shillong
- Mithra Hospital, Bangalore
- Shanthi Hospital and Research Centre, Bangalore
- Sukarya, New Delhi
The study is supported by funding from Social Alpha.